Is gut health the key to treating long covid?
Long covid or post-acute covid syndrome (PACS) is a major health challenge arising from the pandemic. If you have lingering symptoms 12 weeks after an acute Covid-19 infection, you may have long covid.
Research is emerging on the vital role of digestive health and the gut microbiome in this condition. There is a strong association with gut dysbiosis and the persistence of symptoms in long covid. Studies show reduced microbiota diversity, increased opportunistic pathogens and fewer beneficial bacteria to support the immune system.
Read my earlier article Natural Treatment for Long Covid for more details on symptoms.
Gut health as one of the targets of long covid therapy
Naturopaths always say, “All health begins in the gut”. We are now saying, “Long covid persists in the gut”.
The long covid cloud does have a silver lining because gut health is something you can take immediate action to improve. Start with your next meal.
My intention is not to overly simplify what is a complex and debilitating condition. I’ve combined current research plus my clinical experience to provide a starting point. Gut health is a foundation but depending on your circumstances it will be just one of the levers to restore your health. Treatment for these type of conditions usually has many layers.
In this article, I will explore what is happening in the gut and give you some practical strategies and tips to get you started. I will discuss some supplements, but I recommend you work with a practitioner to devise a targeted treatment plan that considers any underlying health conditions and medications.
Long covid is a new condition, so I will update this as more information becomes available from research and real-world clinical experiences in my Naturopathic clinic.
How Covid impacts the gut
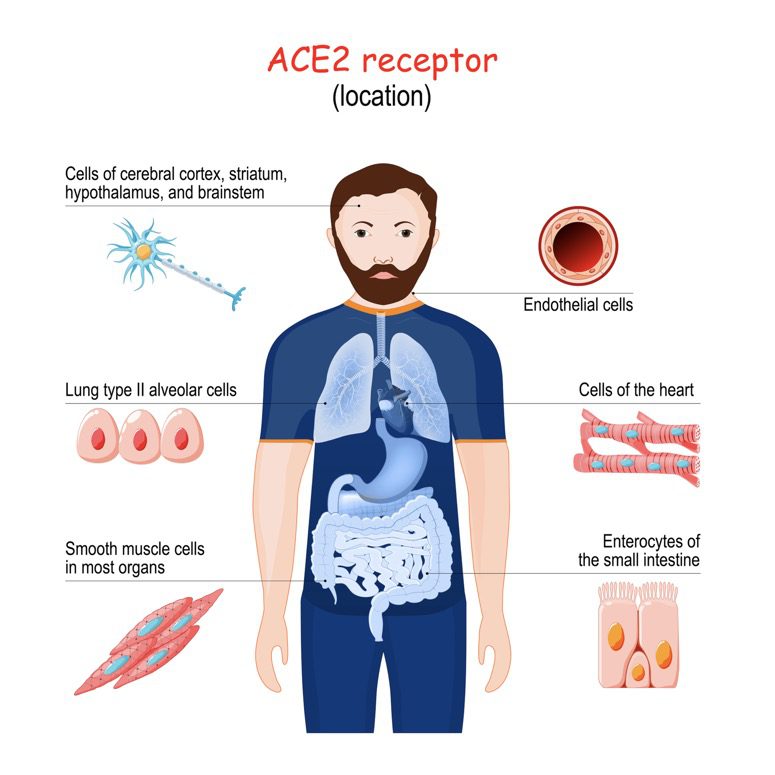
In an acute Covid-19 infection, the SARS-CoV-2 virus spike protein infects our cells via the ACE2 receptor. You’ll find ACE2 receptors throughout the body, many of which are in the gastrointestinal tract (GIT).
ACE2’s role in GIT is to create antimicrobial peptides. These are a natural defence system – kind of like a natural antibiotic. These antimicrobial peptides weed out the undesirable microbes allowing the beneficial ones to thrive. This helps keep the microbiome in a healthy balance.
Covid-19 uses the ACE2 receptor as an entry door to the cell, which then causes ACE2 expression to be downregulated. Less ACE2 equals fewer antimicrobial peptides. This causes a bloom of opportunistic microbes. This imbalance in the gut also affects other systems via the gut-brain, gut-lung, gut-skin axes, and much more. The bad guys outnumber the good guys, and we need the good guys to make things like short-chain fatty acids, hormones and vitamins.
This microbiome imbalance will be much worse if you had dysbiosis/gut issues/chronic inflammatory consitions before the Covid-19 infection.
Effects of an inflamed gut and dysbiotic microbiome
- Increased intestinal permeability. (Leaky gut)
- Increased risk of inflammatory bowel disease
- IBS-like symptoms (changes to bowel motions, constipation/diarrhoea)
- Reduction in immune function and increased susceptibility to infections and risk of developing autoimmune conditions
- Worsening of pre-existing inflammatory conditions such as asthma, metabolic syndrome and Type 1 & 2 diabetes
- Fatigue, brain fog and mood changes (increased anxiety and depression)
- Worsening of skin conditions such as acne, rosacea, and eczema. Development of new skin conditions.
What’s this got to do with long covid symptoms?
As you can see, disruption to the gut ecology/microbiome reaches beyond the gut.
Sub optimal gut function creates or increases the body-wide inflammatory burden. Excess inflammation and immune activation are drivers of long covid.
What happens in the gut does not stay in the gut.
Restoring gut health after covid infection
So now we know how covid affects the gut, what can we do about it? Lots.
The biggest driver of gut health is what you put in your mouth. Diet choices can both help and hinder.
You can begin right now to optimise your diet to
- Reduce inflammation.
- Feed your gut microbiome.
How to use diet to improve your gut microbiome
Changes to the gut microbiome are seen in as little as four days. However, you’ll need to be consistent with your diet to see gradual continued improvement. Don’t expect a quick fix.
Increase fibre
I’m not talking about grey tasteless, processed fibre from a box. What your microbiome craves is plant fibre, both soluble and insoluble. Fruits and vegetables naturally contain both types. You don’t need to worry about the differences between these types because Nature has you covered.
So in simple terms, to promote a healthy microbiome, you need to eat your vegetables.
How much?
Either 600g a day of non-starchy vegetables or, you don’t have scales, 5-7 serves. One serve is one heaped handful of cooked vegetables or a double-heaped handful of raw/salad vegetables.
If your relationship with vegetables has been lacking, gradually increase your level to avoid excess flatulence/gas.
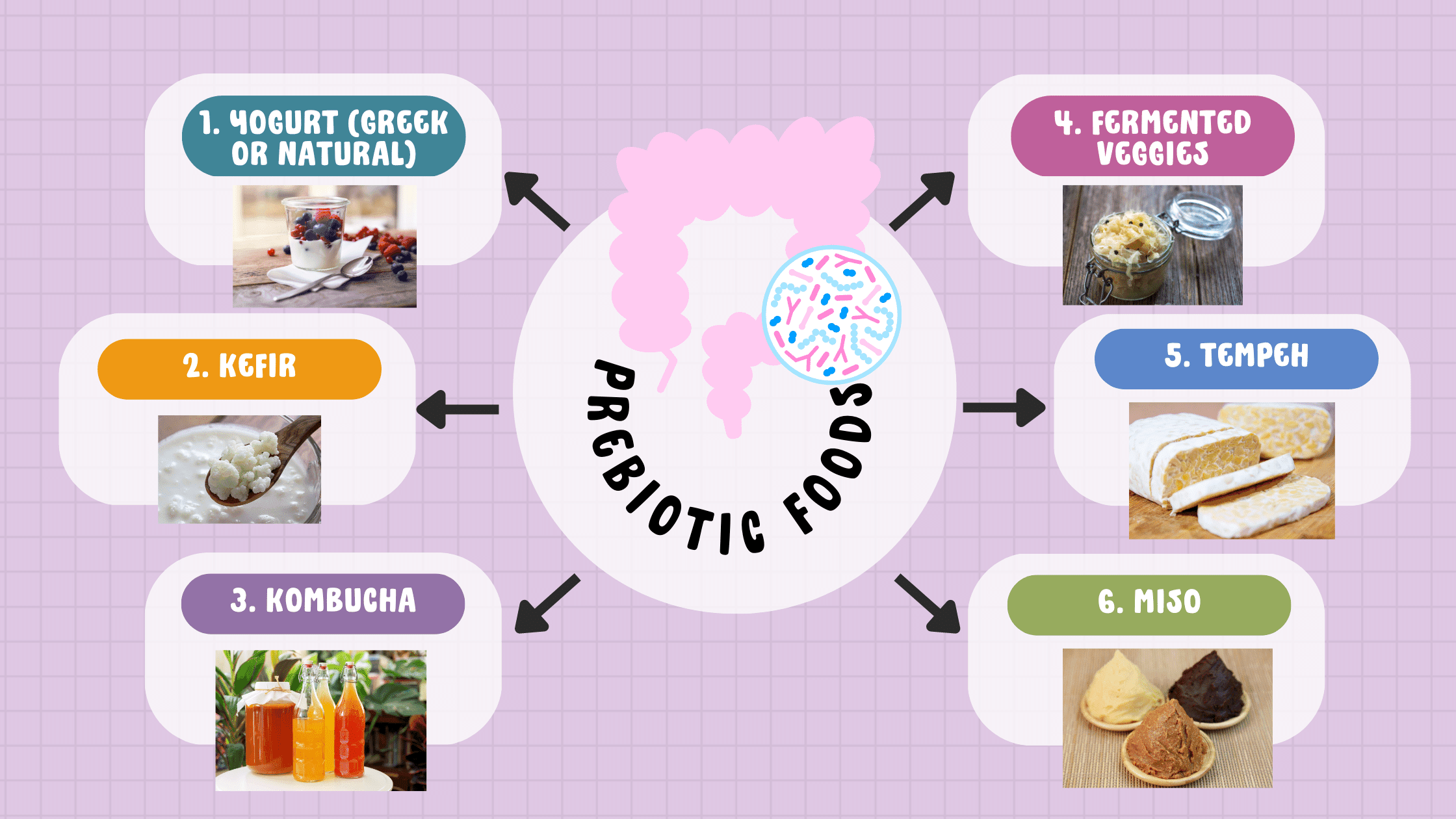
Include prebiotic foods
Prebiotic foods contain small amounts of beneficial bacteria. They can be a helpful addition to your daily diet.
If your gut is highly dysbiotic or inflamed, you might not tolerate these initially. Don’t worry because if you’re getting 600g of veggies, you’re still nourishing your gut bugs.
Include foods high in polyphenols
Polyphenols are natural chemicals plants produce when exposed to stress or pathogens.
When consumed regularly as part of a plant-rich diet, polyphenols can
- Act as a prebiotic enhancing the production of health-promoting Bifidobacterium and Lactobacillus species
- Regulate the gut-brain axis
- Support hormone production
- Maintain the integrity of the intestinal mucous barrier and reduce leaky gut.
Some of the most well-known polyphenols include
- Green tea polyphenols (green tea)
- Resveratrol (dark grapes, berries, soybeans, peanuts, pomegranate)
- Curcumin (Turmeric)
- Quercetin (Onions, grapes, broccoli, apples and berries)
- Cocoa polyphenols (Chocolate)
Green tea polyphenols are the most readily absorbed of the polyphenols.
Quercetin has anti-fatigue and neuroprotective properties supporting recovery from long covid fatigue and brain fog.
Cocoa polyphenols can enhance microcirculation and nitric oxide synthesis to improve vascular function, often impaired in long covid. Does this mean you can eat heaps of chocolate a day? No, a couple of squares of dark chocolate (>70%) will get you the benefits without the detriment of the added refined sugar.
Because polyphenols generally aren’t well absorbed, you should consume them daily.
Resistant starch
Resistant starch is a type of fermentable fibre not digested in the stomach, and small intestine and so arrives in the colon ready to feed your gut microbes.
I’ve written a detailed article on resistant starch which delves into all the benefits.
Resistant starch includes
- Cooked and cooled starchy vegetables like potato and sweet potato. I like to add these to salads or have them as a snack.
- Cooked and cooled rice and pasta.
- Lady finger bananas or green bananas (they have a higher starch-to-sugar ratio)
- Uncooked rolled oats like you’d find in overnight oats recipes.
Reduce your inflammatory burden
Inflammation is a driver of many long covid symptoms. Removing/reducing inflammatory foods from your diet can dramatically impact body-wide inflammation.
These include all the usual suspects.
- Refined sugars (cane sugar, high fructose corn syrup, maltodextrin, sugar alcohols)
- Alcohol
- Highly processed grains (commercial bread, breakfast cereals, instant noodles, pastries, biscuits
- Highly processed seed oils found in commercially processed foods (canola, sunflower)
- Processed meats (ham, bacon, deli-style meats)
- Highly processed foods with preservatives, additives, emulsifiers and thickeners.
The role of gut healing supplements and long covid
Targeted supplementation can be a helpful addition to treating long covid. The emphasis here is on addition. Diet is the foundation. What you eat has the most significant long-term impact, not just long covid but on your overall health.
Probiotics for long covid
So, what do we know about probiotics and long covid? The gut health and immune benefits of probiotics are well known. So regarding supplementation, this is a logical place to start.
There are some small studies at the time of writing but watch this space as I expect to see more research published on this topic.
Cambridge University Hospital researchers used a combination of five strains of Lactobacillus and the prebiotic inulin in a small clinical trial. Participants were given the prebiotic/probiotic supplement for 30 days. Researchers noticed significant improvements in fatigue, digestive symptoms, and self-reported wellbeing. The elderly, those with severe acute infections and those with pre-existing digestive issues saw the most significant benefit.
Another study explored how an oral probiotic combination containing 2.4 billion bacteria consisting of Lactobacillus spp., Bifidobacterium spp. and Streptococcus thermophilus decreased fatigue risk by improving the intestinal production of amino acids and lactate. Lactate is an energy source for the brain and can protect against cognitive dysfunction.
Be cautious though as some people reported feeling worse on self-prescribed probiotics.
Prebiotics for long covid
Unlike probiotics which are actual microorganisms, prebiotics are selective and specific fibres that alter the composition of the intestinal flora and provide a food source for beneficial bacteria to survive.
While probiotics offer benefits while taking them, they don’t change the balance of your microbiome, and the effects diminish within a week of stopping them. Prebiotics, on the other hand, improve the amount and diversity of your microbiome.
Specific research is currently lacking, but prebiotics improve intestinal barrier function as they increase short chain fatty acid (SCFA) production. Some oligosaccrahides can even reduce viral loads, which is a helpful intervention in long covid.
Prebiotics fibres
- Inulin (as used in the study mentioned above)
- Partially hydrolysed guar gum (PHGG)
- Galactooligosaccharides (GOS)
- Banana resistant starch
- Larch arabinogalactans
- Beta-glucans
Prebiotics are less expensive than probiotics (usually about 60% less). However, you might not tolerate some prebiotics if you have pre-existing gastrointestinal inflammation. I usually bring these in later in the treatment plan after diet changes and other strategies to reduce intestinal inflammation.
You can get smaller amounts of most prebiotics through your diet. Chicory root, leeks, asparagus, onions, edamame and oats all contain inulin. Beta-glucans are found in oats.
Sulforaphane
Sulforaphane is a molecule found in cruciferous vegetables. Sulforaphane benefits digestive health by activating the gut’s in-house antibacterial proteins, deactivates lipopolysaccharides on gram-negative bacteria which contribute to body-wide inflammation, improves gut barrier function (reduces leaky gut), decreases inflammation and oxidative stress and destroys biofilms. High-yielding extracts are used as therapeutic nutraceuticals.
Outside of the gut, sulforaphane can support immune function by improving the function of Vitamin D receptors.
Restoring ACE2 function is vital to overcoming many long covid symptoms. Sulforaphane may help restore ACE2 function by increasing sirtuin1 (SIRT1) expression. SIRT 1 is responsible for ACE2 expression. This hasn’t yet had clinical studies in long covid, so it’s theoretical but a potentially beneficial bonus of this nutraceutical.
There are nuances to achieving success with sulforaphane. It won’t be effective if you also use supplementary antioxidants like Vitamins A, C, and E (dietary sources of these are acceptable) or N-acetylcysteine (NAC).
Make diet your ally in long covid recovery
Long covid is a debilitating condition. Support your recovery by improving your gut function, which has many benefits beyond the gut. An anti-inflammatory diet that feeds your microbiome is the foundation for health and can have powerful impacts.
You’ve got to eat anyway, so make it count.
Changes won’t happen overnight, but if you are consistent, you’ll notice gradual and sustained improvements in your symptoms. Think of it as a healthy way of eating to maintain throughout life to increase your resilience and wellbeing.
References available on request.
If you enjoyed this article, you might also like
- Natural treatments for Long Covid
- Natural treatments for Long Covid brain fog
- Health benefits of resistant starch
- 9 of the best whole food sources of Vitamin C

Need help with long covid?
Norelle Hentschel is an experienced Naturopath with a clinic in Stones Corner, South East Brisbane and also offers Telehealth consults Australia wide. She enjoys helping people regain their health.