A Naturopath’s guide to get your period & fertility back
Have you been diagnosed with polycystic ovarian syndrome (PCOS)? Not sure what you can do? Here’s your comprehensive guide to understanding the underlying causes and what natural treatments work for PCOS.
PCOS Defined
PCOS is a female reproductive and metabolic disorder affecting 5-15% of women worldwide1.
PCOS is diagnosed by the presence of two out the three following criteria:
- Elevated androgens
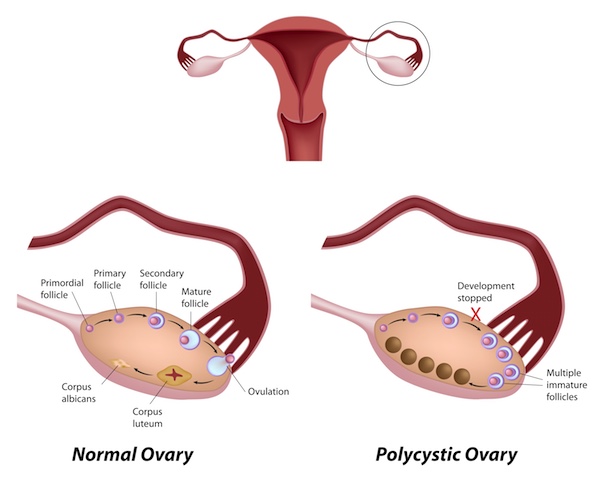
- Polycystic ovaries on ultrasound
- Ovulation abnormalities resulting in irregular periods and infertility2
Among health professionals, there is no consensus on how it develops, and many practitioners consider PCOS a cluster of symptoms rather than a single disease.
Failure to ovulate as a keynote symptom in PCOS
Central to PCOS is the inability to ovulate regularly with menstrual cycles longer than 35 days. Ovulation is the primary way you make progesterone and estrogen. If ovulation does not occur, other hormones like testosterone become unbalanced. High testosterone may cause rouge hair growth (upper lip, abdomen, nipples and sideburns), hair loss on head, acne, weight gain and infertility.
Who gets PCOS?
Because this syndrome is a cluster of symptoms, there is no single presentation.It’s not only overweight women; thin women get PCOS too. Not all will have excess hair growth or acne. To paraphrase Leo Tolstoy: Every woman with PCOS has it in her own unique way.
Choose a customised natural treatment plan
There is a multitude of natural treatment options for PCOS. To determine what will be the most effective you’re going to have to get personal. Work with a qualified practitioner to discover the reason/s why you are not ovulating. Looking at your particular picture and treating this is more effective than using a “one size fits all” PCOS protocol.
What causes PCOS?
PCOS patients present (mostly) in three different ways – insulin resistant, inflammation or post-pill PCOS. There are often overlaps between these types as well.
Insulin-resistant PCOS
Often referred to as “diabetes of the ovaries”, insulin resistance contributes to 60% of PCOS cases3. The biggest culprit is the excess consumption of refined foods and sugar. Hormonal contraception, magnesium deficiency, transfats, smoking, environmental toxins, shift work and sleep deprivation can also contribute.
With insulin resistant PCOS the ovaries produce androgens (testosterone) instead of estrogen and become polycystic.
Insulin resistance PCOS is a risk factor for other metabolic conditions including Type 2 diabetes, heart disease and Non-alcoholic fatty liver disease.
Misconceptions
My fasting blood glucose test is normal – I can’t have insulin resistance.
Wrong – You’ll need a fasting insulin test to discover how hard insulin is working to keep your blood glucose in range.
Only overweight women can have insulin resistant PCOS.
Wrong – Women of all shapes and sizes can have insulin resistance, especially in the early stages.
Treatment ideas
The foundational treatment for insulin resistant PCOS is a healthy diet and regular exercise.
Diet:
Cut out refined sugar, processed foods and transfat. Include vegetables, fruits, good quality protein and healthy fats4. Be alert to healthy food traps like dried fruit and fruit juices which contain high amounts of sugar. A Paleo style diet or intermittent fasting can also be beneficial5.
Some specific diet tips to benefit PCOS
Apple cider vinegar
Apple cider vinegar may improve insulin sensitivity. In a trial of women with PCOS, 57% of those who consumed 20mL of apple cider vinegar per day had a period within 40 days. Testing showed insulin sensitivity improved along with the LH/FSH ratio.
The amount used in this study is achievable as a part of your diet. Use a homemade vinegar salad dressing and ditch the store bought ones which are often high in sugar. 6

Spearmint tea
Swap the coffee for a tea
Spearmint (Mentha spicata) helps to reduce testosterone and hirsutism. Studies have shown a benefit of 2 cups per day over 30 days.7 In summer, spearmint is refreshing as an iced tea.
Cinnamon
Cinnamon has a mild sweet taste which can support the change to a diet lower in refined sugar. One teaspoon of cinnamon sprinkled over your yoghurt, porridge or added to a smoothie can help improve cholesterol levels, insulin sensitivity and increase antioxidant status. Cinnamon improves menstrual cycle regularity in PCOS8.
Exercise
Regular moderate exercise or short duration high-intensity interval training help regulate insulin. Avoid long duration intense activity as this can disrupt hormone balance.
If you are overweight, a 5-10% weight loss helps restore ovulation and regular periods.
Nutrients and herbs
- Peony and liquorice 9 (caution with high blood pressure),
- Gymnema,
- Berberine
- Magnesium,
- Zinc,
- Inositol10
- Chromium11.
Inflammatory PCOS
Inflammatory states cause an increase in cortisol disrupting hormones receptors. Cortisol impairs ovulation by increased production of adrenal androgens (DHEA and androstenedione)12.
Causes of inflammation include:
- Inflammatory diet (sugar, gluten dairy)
- Intestinal permeability or leaky gut
- Chronic infections
- Autoimmune conditions
- Stress (Psychological and physical)
Treatment considerations
- Diet modifications – Remove inflammatory foods especially gluten and dairy
- Put in place stress reduction techniques (relaxation breathing, meditation, gentle exercise, adequate sleep)
- Turmeric13, probiotics, berberine, magnesium, zinc, fish oil14 can all be beneficial.
Post-pill PCOS
Some women regain their cycles within a month or two of stopping the oral contraceptive pill (OCP). Yet, it is not uncommon for your period to take up to 18 months to 2 years to return. The OCP shuts down the hormone signalling pathways. In some women, this takes longer to restore than others, and no one knows why.
Failure to get a cycle back after stopping the pill can be very distressing for women looking to start a family. This is likely to be an underlying cause when women had regular periods before using the OCP.
Give your body some time to kickstart natural hormone production – 3-4 months. A healthy diet and managing stress levels will be significant support here.
Herbal treatment is effective in restoring periods after the pill. Choosing the right herb is complex. Work with a Naturopath or herbalist who can interpret your test results and symptoms. Vitex is often misused here and may make things worse.
When it may not be PCOS
Other reasons for lack of ovulation
Low body fat
Women doing intense physical activities or consuming insufficient calories will have low body fat. The body perceives this as stress and hits the pause button on the part of your brain that sends signals to make hormones.
From an evolutionary perspective, this was important during times of famine. Restoring ovulation in these situations is about increasing body fat. A body fat percentage of at least 18% restores fertility.
Hypothyroidism
Low thyroid function decreases the production of follicle stimulating and luteinizing hormone which can impair ovulation 15. Investigate further if you Thyroid stimulating hormone (TSH) result is higher than 2.5.
Zinc deficiency
Healthy ovulation needs zinc. This is a nutrient often low in vegetarian and vegan diets. The OCP also depletes this mineral.
Iodine deficiency
Aside from your thyroid, your ovaries also need enough iodine to promote ovulation. Always test iodine before you supplement as too much can be as bad as not enough.
What tests should you get for PCOS?
As part of the testing for PCOS don’t rely just on an ovarian ultrasound. Here are some other investigations that your doctor or Naturopath can order.
- Follicle stimulating hormone
- Luteinizing hormone
- Prolactin
- Fasting Blood glucose
- Fasting insulin
- Testosterone
- Sex Hormone Binding Globulin
- DHEA
- Androstenedione
- Thyroid stimulating hormone (and possibly further thyroid tests)
- Urinary iodine
Is PCOS curable?
Unlike puppies, PCOS does not have to be for life. As women’s health expert and author Lara Briden says:
“Know when it’s time to let go of your PCOS Diagnosis. In most cases, PCOS is not a permanent condition. With the right diagnosis and the proper treatment, PCOS can become a thing of the past.”
How long will PCOS treatment take?
The average time for improvement is around 6-9 months. Some women can get regular cycles back in three months.
Want help finding your natural PCOS treatment?
Are you ready say goodbye to PCOS? Get your hormones happy and balanced? Enhance your fertility? There are many approaches to PCOS treatment.
Avoid having a pantry shelf full of supplements. Book in for a consult. Get professional guidance for your personalised, natural PCOS treatment plan.
** It is essential to work with a qualified practitioner if you are planning on using herbal medicines or nutritional supplements. If you are on medication or have an existing medical condition, some herbs and supplements may not be suitable.
References:
- Bednarska S, Siejka A. The pathogenesis and treatment of polycystic ovary syndrome : What ’ s new ? Adv Clin Med. 2017;26(2):359-367. doi:10.17219/acem/59380.
- Yau TTL, Ng NYH, Cheung LP, Ma RCW. Polycystic ovary syndrome : a common reproductive syndrome with long-term metabolic consequences. Hong Kong Med J. 2017;23(6):622-634. doi:10.12809/hkmj176308.
- Rosenfield RL, Ehrmann DA, Biochemical A. The Pathogenesis of Polycystic Ovary Syndrome ( PCOS ): The Hypothesis of PCOS as Functional Ovarian Hyperandrogenism revealed. Endocr Rev. 2018;37(October 2016):467-520. doi:10.1210/er.2015-1104.
- Marsh K a, Steinbeck KS, Atkinson FS, Petocz P, Brand-Miller JC. Effect of a low glycemic index compared with a conventional healthy diet on polycystic ovary syndrome. Am J Clin Nutr. 2010;92:83-92. doi:10.3945/ajcn.2010.29261.Am.
- Chiofalo B, Simone A, Palmara V, et al. Fasting as possible complementary approach for polycystic ovary syndrome : Hope or hype ? Med Hypotheses. 2017;105:1-3. doi:10.1016/j.mehy.2017.06.013.
- Wu D, Kimura F, Takashima A, et al. Intake of Vinegar Beverage Is Associated with Restoration of Ovulatory Function in Women with Polycystic Ovary Syndrome. Tohoku J Exp Med. 2013;230(1):17-23. doi:10.1620/tjem.230.17.
- Grant P, Ramasamy S. An update on plant derived anti-androgens. Int J Endocrinol Metab. 2012;10(2):497-502. doi:10.5812/ijem.3644.
- Kort DH, Lobo RA. Preliminary evidence that cinnamon improves menstrual cyclicity in women with polycystic ovary syndrome : a randomized controlled trial. Am J Obstet Gynecol. 2014;211(5):487.e1-487.e6. doi:10.1016/j.ajog.2014.05.009.
- Arentz S, Smith CA, Abbott J, Fahey P, Cheema BS, Bensoussan A. Combined Lifestyle and Herbal Medicine in Overweight Women with Polycystic Ovary Syndrome ( PCOS ): A Randomized Controlled Trial. Phytotherpay Res. 2017;1340(March):1330-1340. doi:10.1002/ptr.5858.
- Unfer V, Facchinetti F, Orrù B, Giordani B, Nestler J. Myo-inositol effects in women with PCOS : a meta-analysis of randomized controlled trials. Endocr Connect. 2017;6:647-658. doi:10.1530/EC-17-0243.
- Hywood A. Phytotherapy for PCOS. Aust J Herb Med 2012. 2012;24(3). http://www.nhaa.org.au/docs/AJMH/Aust_J_Herbal_Med_243_September_2012.pdf.
- Paschou SA, Paschou SA, Palioura E, Ioannidis D. Adrenal hyperandrogenism does not deteriorate insulin resistance and lipid profile in women with PCOS. Endocr Connect. 2017;6:601-606. doi:10.1530/EC-17-0239.
- Mohammadi S, Kayedpoor P, Karimzadeh-bardei L, Nabiuni M. The Effect of Curcumin on TNF- α , IL-6 and CRP Expression in a Model of Polycystic Ovary Syndrome as an Inflammation State. J Reprod Infertil. 2017;18(4):352-360.
- Yang K, Zeng L, Bao T, Ge J. Effectiveness of Omega-3 fatty acid for polycystic ovary syndrome : a systematic review and meta-analysis. Reprod Biol Endocrinol. 2018;16(27):1-13.
- Neema A, Sourya A, Samarth S. Gonadotropin Levels in Hypothyroid Women of Reproductive Age Group. J Obs Gynecol India. 2011;61(October):550-553. doi:10.1007/s13224-011-0079-7.

Need help with your PCOS treatment plan?
Norelle Hentschel is an experienced Naturopath with a clinic in Stones Corner, Brisbane who enjoys supporting her clients to reach their health goals.
Want more articles like this?
Receive a monthly digest of natural health information to help you become “health” sufficient!
PS. Your inbox real estate is precious, and we will never annoy you with sales pitches or share your details with anyone else. One email a month — that’s it.

