Quick answer
Supporting gut health may help reduce psoriasis flare frequency and severity by influencing immune activity and systemic inflammation, but it does not cure psoriasis.
Psoriasis is often experienced on the skin, but for many people it doesn’t feel skin‑deep. Flare‑ups can coincide with digestive issues, food reactions, stress, illness, or antibiotic use. These are all clues that the gut and immune system may be involved.
While psoriasis has a genetic and immune component, growing research suggests the gut–skin connection may influence inflammation, immune signalling and symptom severity. This doesn’t mean gut issues cause psoriasis, but they can play an important role in how the condition shows up and how well it responds to treatment.
As a naturopath working with people with psoriasis in Brisbane, I see gut health as one part of a broader, personalised management plan — alongside skin care, stress support and nutritional strategies.
Psoriasis and the role of gut health
Psoriasis is a chronic inflammatory condition influenced by immune activity. Research suggests the gut microbiome may affect systemic inflammation and immune signalling, which can influence psoriasis severity and flare frequency. Supporting gut health may improve symptom management for some people, and complements standard medical care.
The link between gut health and psoriasis
Although psoriasis has a genetic component, there is also growing evidence of a strong link between symptom severity and digestive health. People with psoriasis have demonstrated decreased bacterial diversity, bacterial overgrowth in the small intestine (SIBO), and increased intestinal permeability (leaky gut).
They may also have sluggish liver function and a deficiency of bile acids, which are needed to absorb dietary fats and fat-soluble vitamins like A, D, E, and K (1). Some people with psoriasis also experience inflammatory bowel diseases such as Crohn’s disease and Ulcerative Colitis.
The visible signs of psoriasis are on the skin, but evidence suggests that the gut microbiome’s composition can influence disease severity through immune modulation. What’s the connection?
The gut impacts the skin via the “Gut-skin axis”. This is a two-way communication between the gut and the skin mediated by the immune system.
👉🏻 Curious how your gut microbiome maps to your skin symptoms? Learn more about microbiome testing.
The science behind the gut-skin connection
Gut dysbiosis in psoriasis
People with psoriasis tend to have a gut microbiome that is less diverse and more prone to inflammation. This imbalance can weaken the gut lining, allowing harmful substances into the bloodstream (leaky gut) and overstimulate the immune system, all of which can trigger or worsen psoriasis symptoms. The beneficial Akkermansia muciniphilia, Lachnospira, and Faecalbacterium species often decrease, while the inflammation-promoting Escherichia and Ruminococcus species are increased.
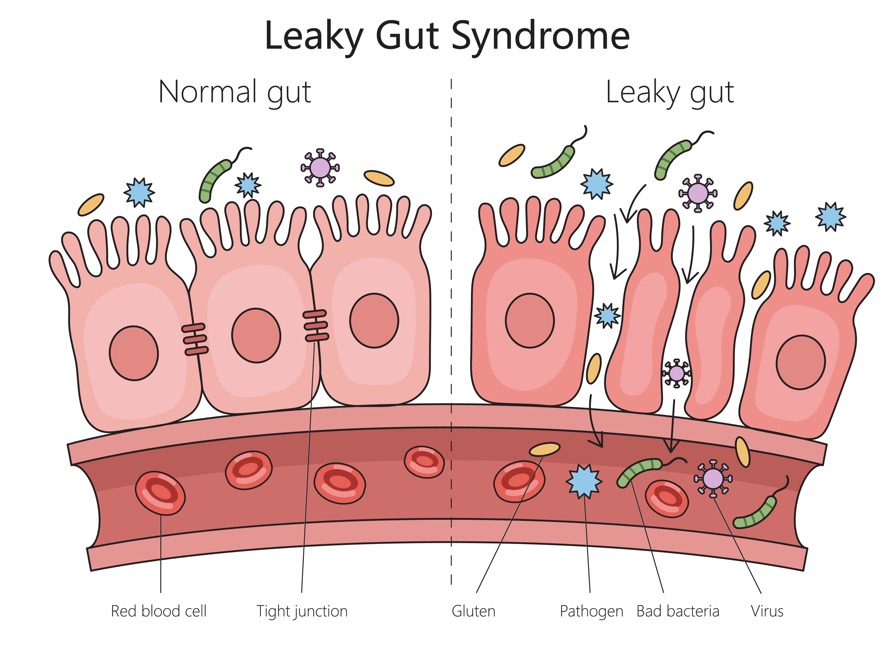
The role of leaky gut in psoriasis
Leaky gut or intestinal permeability is when the tight junctions that form the barrier between the digestive system and the rest of the body allow bacterial toxins to enter the bloodstream. These toxins trigger inflammation and disruption of other body systems, including the skin. For example, the Clostridia species produces metabolites, p-cresol and phenols. These enter the bloodstream and accumulate on the skin, causing dryness, reduced skin barrier integrity and dysregulation of keratinocytes, which are responsible for psoriatic plaques. Clostridia species can become dominant in the microbiome after courses of broad-spectrum antibiotics. Skin tests in psoriasis patients show a high percentage of gut bacterial antigens (2).
Lipopolysaccharides (LPS) are components of bacterial cell walls with dual effects. A-LPS, produced from beneficial bacteria, helps maintain gut health and reduce inflammation, whereas their evil twin, P-LPS, are endotoxins that, in the presence of intestinal permeability, cause systemic inflammation due to alterations in blood glucose regulation and cholesterol metabolism. In psoriasis, A-LPS triggers keratinocytes to go into overdrive and form psoriatic plaques (3).
Immune system cross-talk
A common theme across research studies is that psoriasis patients show reductions in beneficial Akkermansia muciniphilia and Faecalibacterium prausnitzii. These two species produce short-chain fatty acids (SCFA), which support healthy immune system balance via their effect on immune T regulatory (Treg) cells. Imbalanced T-reg cells release inflammatory molecules (cytokines), stimulating skin cells (keratinocytes) to go into overdrive, resulting in psoriatic lesions.
Common gut related patterns seen in psoriasis
Everyone is different, but some patterns frequently show up in clinic:
- Digestive symptoms such as bloating, reflux, constipation or diarrhoea
- A history of frequent antibiotics or gut infections
- Food sensitivities (especially to gluten, dairy or highly processed foods)
- High stress levels or disrupted sleep
- Co‑existing conditions such as IBS, fatigue or joint pain
Addressing these factors doesn’t replace medical care but it can significantly support overall outcomes.
Evidence-informed ways to support gut health in psoriasis
Although psoriasis has traditionally been treated as a skin disease, its systemic immune and inflammatory aspects are now widely acknowledged. Newer medical biologic treatments such as Adalimumab (Humira) target immune inflammation after it occurs. What if we looked to stop the inflammation before it happens by addressing the root causes in the gut microbiome?
Diet, lifestyle, and genetics are key regulators of gut microbiome makeup. While genetics are fixed and unchangeable, we can target diet and lifestyle factors to improve the health of people with psoriasis. Understanding how the gut microbiome regulates skin health offers new, accessible and affordable psoriasis treatment options.
Naturopathic treatment aims
- Reduce inflammation and support a healthy intestinal barrier
- Support the growth of beneficial microbes
- Remove any pathogens and reduce the overgrowth of opportunistic bacteria
Diet – building a psoriasis-friendly gut
Reduce inflammatory foods
- Refined sugars **This does not include whole fruits!!
- Saturated animal fats. Choose lean cuts of meats and include dairy in moderate amounts if tolerated.
- Deep fried foods
- Ultra-processed foods
- Alcohol
Address food intolerances
Some, but not all, people with psoriasis have intolerances to certain components of otherwise healthy foods. These can include vegetables from the nightshade family (potatoes, tomatoes, eggplant, capsicum, chilli, and Gogi berries), gluten, and dairy.
Coeliac disease is up to three times more likely in those with psoriasis. Even if not symptomatic, I advise my psoriasis patients to be screened for coeliac disease (4).
Boost healthy microbes
The overarching strategy is to increase fibre and polyphenols, which provide food for beneficial bacteria. The best source of these is plants, so include a wide variety of in-season fruits and vegetables, plus legumes and pulses. Aim to get the bulk of your fibre from whole food sources rather than supplements, as you get the bonus of all the vitamins and minerals as well.
Boosting Akkermansia muciniphilia and Faecalibacterium prausnitzii
As these two microbes are the most depleted in psoriasis, here are specific dietary strategies to increase their abundance.
Food to increase Faecalibacterium prausnitzii
- Fruits – apples, bananas, berries, oranges, pears
- Vegetables– leafy greens, broccoli, carrots, cauliflower, Brussels sprouts
- Whole grains – oats, barley, brown rice, whole wheat
- Legumes – beans, lentils, chickpeas
- Nuts and seeds – almonds, walnuts, flaxseeds, chia seeds
- Prebiotic foods – chicory root, garlic, onions, leeks, asparagus, bananas, oats
- Polyphenol-rich foods – berries, apples, citrus fruits, grapes, green tea, cocoa
Foods to increase Akkermansia muciniphilia
- Polyphenol-rich foods – apples, berries, grapes, cocoa, green tea, coffee, dark chocolate, plums, olives
- Prebiotic fibres – asparagus, bananas, barley, chicory root, dandelion greens, flaxseeds, garlic, leeks, Jerusalem artichoke, jicama root, oats, onions, seaweed, soybean, wheat bran
- Other plant-based foods ; yams, agave, Brussels sprouts, okra, cauliflower, broccoli
- Healthy fats – Foods rich in omega-3s (fish oil, flax seeds, hemp seeds, olives) may also help.
There is also observational evidence that a Mediterranean-style diet reduces the severity of psoriasis. The above foods are consumed as part of this dietary pattern (5).
Lifestyle changes to support skin and gut health
Stress management
Clinically, people with psoriasis often notice that stress leads to more frequent, severe, and longer-lasting flare-ups. Stress exacerbates psoriasis by altering the gut microbiome, over-activating stress-response systems, weakening anti-inflammatory controls, and boosting skin inflammation.
Over time, this can lead to a cycle where stress worsens gut health, and gut problems increase feelings of anxiety. By practising stress management techniques such as relaxation exercises, mindfulness, or meditation, you help your body return to a relaxed state, reduce flare severity, and improve your quality of life.
Sleep optimisation
Getting enough restorative sleep is vital for a healthy microbiome in four ways.
- Promotes microbial diversity
- Good sleep quality and sufficient sleep duration are associated with higher gut microbiome diversity, a key marker of gut health. People who sleep well tend to have more beneficial bacteria, such as Faecalibacterium prausnitzii and Bifidobacterium, which are linked to reduced inflammation and better gut barrier function.
- Regulates gut-brain axis and circadian rhythms
- Healthy sleep helps maintain the gut-brain axis- a communication network between the gut and brain that relies on nerves, hormones, and immune signals. This axis is crucial for regulating sleep cycles and gut function. Gut bacteria follow circadian rhythms, and sleep disruptions can throw off these microbial cycles, leading to imbalances and increased inflammation.
- Supports production of key metabolites
- Sleep helps sustain the production of short-chain fatty acids (SCFAs) like butyrate, acetate, and propionate, which are essential for gut barrier integrity and inflammation control. Poor sleep reduces SCFA production, increasing the risk of a “leaky gut” and systemic inflammation.
- Reduces Inflammation
- Consistent, restful sleep helps keep pro-inflammatory cytokines (such as IL-6 and TNF-α) in check, supporting a healthier gut environment[4]. Sleep deprivation, on the other hand, increases these cytokines, harming the gut lining, the microbiome and the skin.
Start getting your sleep back on track by implementing this simple 2-step evening routine.
Herbal and natural remedies
Although diet and lifestyle are the foundations of a healthy gut-skin connection, sometimes additional support can help you gain more traction. When it comes to supplements, personalised treatment plans get the best results for my clients rather than generic, cookie-cutter protocols. That’s why I recommend consulting with a qualified practitioner to ensure you get the best and safest prescription for you, especially if you are taking prescription medication, are pregnant, or are breastfeeding.
However, not everyone can access a naturopath or herbalist, so here are some researched supplements you might want to consider.
Turmeric
Turmeric and its polyphenol, curcumin, have been shown to promote microbial diversity and reduce LPS-producing bacteria and leaky gut (6). Studies have shown that turmeric’s anti-inflammatory and antiproliferative actions significantly reduced the Psoriasis Area Severity Index (PASI) (7).
Prebiotics
Prebiotic fibres like partially hydrolysed guar gum (PHGG) and inulin have been shown to favourably alter the composition and activity of the microbiome, specifically improving the abundance of Akkermansia species by up to five times (8).
Probiotics
The probiotic Lactobacillus paracaesi CNM-2116 (STII) has reduced skin inflammation and improved skin barrier function in clinical trials (2). A 12-week randomised controlled trial using a multi-strain probiotic containing Bifidobacterium longum CECT 7347, Bifidobacterium lactis CECT 8145, and Lactobacillus rhamnosus CECT 8361 showed an up to 75% reduction in PASI scores with fewer flares at the six-month follow-up (9).
Sulforaphane
Sulforaphane (SFN) is derived from broccoli sprouts. It acts primarily by activating the Nrf2 (nuclear factor erythroid 2-related factor 2) signalling pathway. This activation enhances the production of antioxidant and detoxification enzymes, which bolsters the gut’s antioxidant defences. By reducing oxidative stress and inflammation, SFN can prevent gut barrier dysfunction (i.e., leaky gut) and dysbiosis.
Microbiome testing in psoriasis
The rise and affordability of direct-to-consumer microbiome testing provide insights into your microbiome and allow more personalised and targeted prescriptions. While it’s not essential, it can be a useful tool, especially in more complex cases.
Case Studies and Success Stories
Switching to the Mediterranean diet avoided methotrexate
A 52-year-old male who had large areas of arms and legs with plaques and psoriatic arthritis for the last 15 years wanted to avoid going on methotrexate. He changed to Mediterranean diet, focusing on getting 600g of non-starchy vegetables daily and swapping butter for olive oil. He also reduced alcohol consumption significantly. After 6 months, he had an 80% reduction in the plaques, no symptoms of psoriatic arthritis, and no need for pharmaceutical medication.
Post-infectious psoriasis flare
A 39-year-old female had a history of mild, intermittent scalp psoriasis since her teenage years. After a bout of bad gastroenteritis, treated with antibiotics, the psoriasis worsened. Microbiome testing revealed some opportunistic bacterial overgrowth and depleted Akkermansia species. A three-month treatment program focusing on increasing dietary polyphenols, supplementing with PHGG, and using a custom liquid herbal blend saw the scalp totally clear of lesions.
The outcomes presented in these case studies reflect one person’s experience only and are not guaranteed or typical. Results will vary depending on individual circumstances. This information is provided for educational purposes and is not intended as medical advice or a substitute for personalised healthcare assessment.
Next steps
In summary, addressing the gut-skin connection represents a powerful, evidence-based approach to managing psoriasis. By targeting gut health through dietary changes, probiotics, and lifestyle interventions, we can reduce inflammation, support immune balance, and strengthen the intestinal barrier, all of which have been shown to significantly improve psoriasis symptoms and overall quality of life. Research consistently demonstrates that restoring microbial balance in the gut alleviates skin flare-ups and offers a safer, more holistic path to long-term skin health.
Book an appointment today if you’re ready to take control of your psoriasis from the inside out. Together, we can create a personalised plan to heal your gut, calm your skin, and help you feel your best.
Further reading
- Gut health benefits of resistant starch – your ultimate guide
- How to protect and repair your gut while on antibiotics
- Topical herbal treatments for psoriasis
References
- Ely PH. Is psoriasis a bowel disease? Successful treatment with bile acids and bioflavonoids suggests it is. Clin Dermatol. 2018;36(3) 76–89.
- Thye AYK, Bah YR, Law JWF, Tan LTH, He YW, Wong SH, et al. Gut-Skin Axis Unravelling the Connection between the Gut Microbiome and Psoriasis. Biomedicines. 2022 Apr 30;10(5) 1037.
- Gyurcsovics K, Bertók L. Pathophysiology of psoriasis – coping endotoxins with bile acid therapy. Pathophysiology. 2003 Dec 1;10(1) 57–61.
- Ungprasert P, Wijarnpreecha K, Kittanamongkolchai W. Psoriasis and Risk of Celiac Disease – A Systematic Review and Meta-analysis. Indian J Dermatol. 2017;62(1)41–6.
- Perez-Bootello J, Berna-Rico E, Abbad-Jaime de Aragon C, Cova-Martin R, Goni L, Ballester-Martinez A, et al. Impact of the Mediterranean Diet on Patients With Psoriasis – Protocol for a Randomized Controlled Trial. JMIR Res Protoc. 2025 Jan 29;14 e64277.
- Zhu J, He L. The Modulatory Effects of Curcumin on the Gut Microbiota – A Potential Strategy for Disease Treatment and Health Promotion. Microorganisms. 2024 Apr;12(4) 642.
- Antiga E, Bonciolini V, Volpi W, Del Bianco E, Caproni M. Oral Curcumin (Meriva) Is Effective as an Adjuvant Treatment and Is Able to Reduce IL-22 Serum Levels in Patients with Psoriasis Vulgaris. BioMed Res Int. 2015;2015(1) 283634.
- Vandeputte D, Falony G, Vieira-Silva S, Wang J, Sailer M, Theis S, et al. Prebiotic inulin-type fructans induce specific changes in the human gut microbiota. Gut. 2017 Nov 1;66(11) 1968–74.
- Navarro-López V, Martínez-Andrés A, Ramírez-Boscá A, Ruzafa-Costas B, Núñez-Delegido E, Carrión-Gutiérrez MA, et al. Efficacy and Safety of Oral Administration of a Mixture of Probiotic Strains in Patients with Psoriasis – A Randomized Controlled Clinical Trial. Acta Derm Venereol. 2019 Nov 1;99(12) 1078–84.
Frequently asked questions about psoriasis and gut health
Can gut health really affect psoriasis?
Yes. Research suggests changes in the gut microbiome may influence immune pathways involved in psoriasis. Gut health does not cause psoriasis, but it may affect inflammation levels and flare severity.
Does leaky gut cause psoriasis?
No. Psoriasis is an immune‑mediated condition with genetic and environmental factors. Increased intestinal permeability (often called leaky gut) may contribute to systemic inflammation, which can worsen symptoms in some people.
What foods are best for gut health in psoriasis?
There is no single psoriasis diet. Many people benefit from a whole‑food, anti‑inflammatory approach that supports gut bacteria while reducing highly processed foods. Individual responses vary.
Are probiotics helpful for psoriasis?
Some probiotic strains may support immune balance and gut health, but responses are individual. Probiotics should be selected based on symptoms, history and tolerance.
When should I see a Naturopath for psoriasis?
If psoriasis flares are frequent, slow to respond to treatment, or accompanied by digestive symptoms, working with a qualified naturopath may help identify contributing factors and supportive strategies.
What are your qualifications of your naturopaths?
Norelle Hentschel hold an undergraduate Bachelor of Health Science (Naturopathy) and a post graduate Master of Advanced Naturopathic Medicine. I am a professional member of the Australian Naturopathic Practitioners Association (ANPA) which requires me to hold all appropriate insurances and complete on-going professional development education to ensure my care aligns with current best practice.
How much does a psoriasis naturopathic consultation cost?
Consultation fees are transparent and available before booking. Fees are for consults only. Any products purchased from the dispensary are an additional cost.
The current consultation fees can be found on the Book a consult page. Naturopathy is not covered by Medicare. Some private health insurance funds offer rebates for Naturopathy. Check with your fund for details.
If you want more information before booking I also offer a free Discovery Call.

Psoriasis support at Your Remedy Naturopathy (Brisbane)
Norelle Hentschel is an experienced skin Naturopath with a clinic in Stones Corner, Brisbane and Telehealth consults Australia-wide.
Her psoriasis treatments focus on personalised gut and immune support, evidence‑informed nutrition and herbal medicine to address triggers while supporting skin healing.
Book a consultation to explore whether gut‑focused psoriasis support may be appropriate for you.
Want more articles like this?
Join us at Your Skin Remedy – the monthly missive for healthy skin from the inside out. Practical, actionable, and informative. Your clear, glowing skin starts here.
PS. Your inbox real estate is precious. Your Skin Remedy is pitch and promo free. I promise. One email a month — that’s it.
Clinical review and authorship
This page has been written and reviewed by Norelle Hentschel (Master of Advanced Naturopathic Medicine) a degree-qualified naturopath based in Brisbane.
Content is informed by traditional naturopathic principles, current nutrition and skin health research, and over a decade of clinical experience.
Information provided is for educational purposes and does not replace medical diagnosis or treatment. Individual care plans are tailored in collaboration with your healthcare team where appropriate.
Last reviewed on 10 February 2026